Recency of practice is an important concern for medical practitioners in Australia. It’s something you must address both when you register with the Medical Board of Australia for the first time, as well as each time you apply for re-registration. Most doctors tend to focus on the Medical Board standard in relation to recency of practice. But you will also find that most employers have their own expectations and standards around recency of practice. In this post, I am going to guide you through what you need to know about recency of practice, so that you can be appropriately addressing this issue both with the Medical Board as well as with employers.
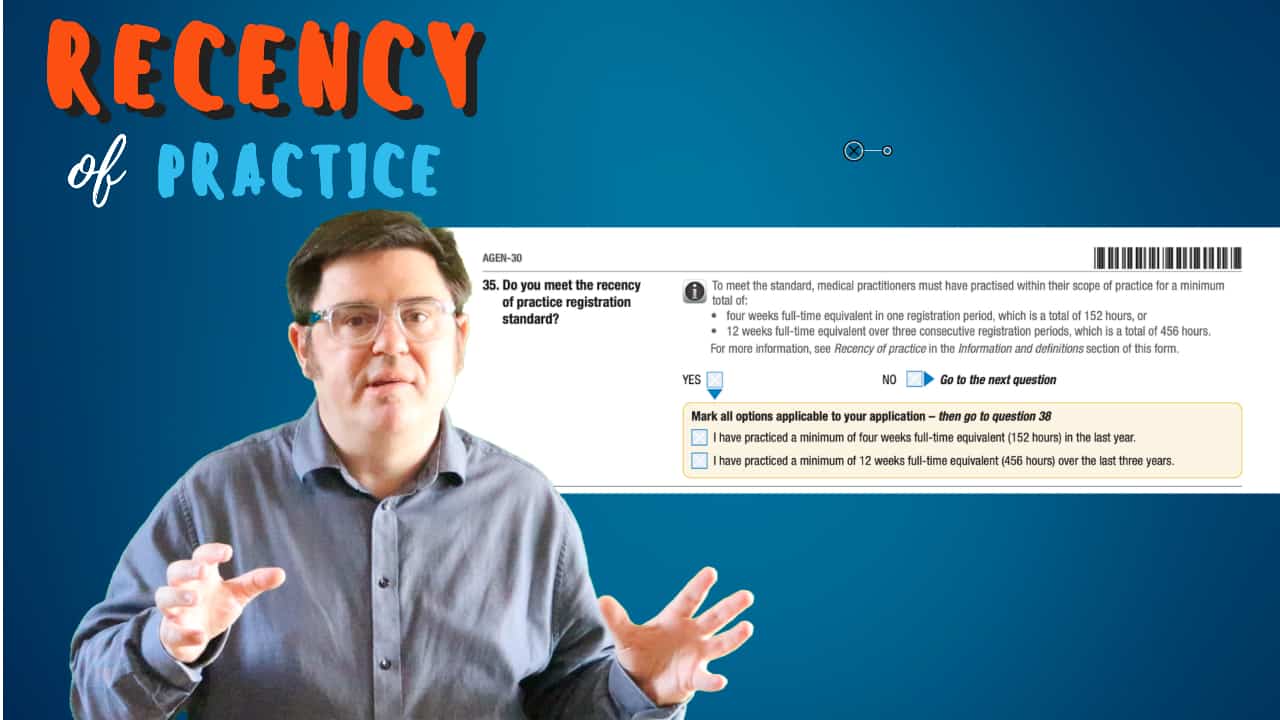
So, firstly let us define what we mean by recency of practice for doctors in Australia. According to the Medical Board of Australia, every registered medical practitioner is required to demonstrate recency of practice, which is defined as working a minimum amount of four weeks full time within your scope of practice in one year (one registration period) or 12 weeks full time within your scope of practice across 3 years (3 registration periods).
From an employment perspective, whilst employers need to be mindful of the Medical Board standard they will generally apply their own standards. A good rule of thumb is if it has been more than 2 or 3 years since you have done a significant amount of clinical work this may be seen as a negative by a prospective employer.
So, in the rest of this post, we will discuss some of the finer details of the recency practice standard, what might happen if you are found to not be recent enough in practice as well as the options for addressing recency of practice from both a Medical Board as well as employer perspective.
Why have a recency of practice standard?
It is important that doctors remain current in the type of clinical medicine that they practice. Most laypeople would consider a situation where a doctor had for example not practiced medicine at all for 5 years and not engaged in any continuing professional development during this time as one where such a doctor may pose a risk to the public if they were to return to clinical medicine with no initial support or oversight.
The question, therefore, is how much recency of practice is enough? Interestingly the Australian Health Practitioner’s Regulation Agency (AHPRA) which oversights the National Boards, including the Medical Board, has reviewed this question a few times. In their most recent report they comment that:
Research undertaken for this and previous reviews of the ROP registration standards did not provide a definitive answer to the question of how much recent practice a health practitioner needs to maintain their skills and knowledge, or whether minimum hours to maintain competence vary according to the profession, type and scope of practice. National Boards have drawn on the research that is available as well as their regulatory experience and the experience of other National Boards to set requirements for recent practice.
AHPRA 2019 Report
They concluded that the revised registration standards balance public safety versus the regulatory burden of allowing practitioners some level of flexibility in their working arrangements.
Scope is just as important as recency.
It is important to note that the Medical Board still expects doctors to recognise their own limitations. Even if they have met the recency of practice requirements they should still consider if what they are doing is within their current scope of practice or whether they should be self-limiting themselves or engaging in further training, assessment, and oversight.
Scope of practice can be a bit difficult to define at times. The Medical Board of Australia defines it as follows:
Scope of practice means the professional role and services that an individual health practitioner is trained, qualified and competent to perform.
Medical Board Australia
Most specialty colleges, for example, will have a statement on their website in relation to the type of clinical practice that they consider a Fellow of the college can safely engage in as a current Fellow of that college.
If you are working as an International Medical Graduate in Australia you may have some limits on your (scope of) practice imposed as part of your registration by the Medical Board. Typically these may be about only working in a particular area of medicine or only working in certain locations where supervision has been approved.
How do you prove recency of practice with the Medical Board of Australia?
Primarily and initially it’s an honesty system. Whenever you apply for registration or a new form of registration or apply to re-register you must indicate to the Medical Board that you meet the recency of practice standard.
The Medical Board does, however, expect that you keep a record of evidence to prove your recency of practice. And also indicates that it does from time to time audit for compliance and will look into your recency of practice further if it receives a notification about you.
What can happen if I give the wrong information to the Medical Board about my recency of practice?
In confirming your recency of practice you are confirming that you comply with the law. Deliberately lying about your recency of practice therefore can have serious consequences if you are found out. Even if you were not deliberately attempting to lie about your recency of practice if it turns out that you were non-compliant you could be in trouble.
What happens to my registration if I am not recent enough in my practice?
If you don’t meet the recency of practice standard then the Board can impose conditions on your registration or refuse your registration.
It is up to you to provide information to the Medical Board to help it decide whether you can safely continue with your registration.
Requirements for medical practitioners with non-practising registration or medical practitioners who are not registered and wish to return to practice (includes international medical graduates).
| Have had 2 or more years of clinical experience | Not practising for up to 12 months | No additional requirements to be met |
| Have had 2 or more years of clinical experience | Not practising for between 12 months and 3 years | Before re-commencing must complete the equivalent of 1 year’s relevant CPD |
| Have had 2 or more years of clinical experience | Not practising for more than 3 years | Need to provide a plan for professional development and re-entry into practice |
| Have had less than 2 years of clinical experience | Not practising for more than 12 months | Required to recommence in a supervised training position |
REGISTRATION STANDARD:
Recency of practice
1 October 2016
For those doctors who are required to catch up with Continuing Professional Development the easiest path for doing this is via a college CPD program if you are a member of such a college. Many IMGs will register with the RACGP for this purpose, although it should be noted that RACPG CPD is technically only relevant to general practice and not hospital medicine, although clearly there is overlap.
If you have been out for more than 3 years and are a member of a college then you will normally find that the college provides a re-entry program option that will satisfy the Medical Board requirement. Generally, this will involve working under the oversight of a college fellow for a period of time.
What if I am changing scope of practice?
Again according to the Medical Board, if you are changing your field or scope of practice, you may need to undertake further training to ensure your competency.
If the change is to a subset of your current practice, i.e. you are narrowing your current practice, there are no additional requirements.
If you are changing your practice in a way that your peers might view as requiring you to undertake more training or you are changing to an entirely different field of practice then you will be required by the Medical Board to consult with the relevant specialist college to develop a professional development plan before entering the new field of practice.
Why do employers have a different interpretation of recency of practice?
Employers are of course obliged to take the Medical Board recency of practice standards into account when considering applicants for job positions. However, employers can and often do make their own interpretations around recency of practice.
Because working supervised is an option for addressing issues around recency of practice employers may consider doctors for posts where the doctors have been out of practice for significant periods.
However, it is my experience, particularly when it comes to trainee positions and international medical graduates that employers are unlikely to see large gaps in clinical practice favourably. Employers usually have several applications to consider and they will tend to take the easier path of employing a doctor who is either just moving between jobs or has 2 years or less time out of medicine.
What are the options for addressing recency of medical practice?
Option 1. Work under supervision to obtain recency of practice
As the Medical Board itself indicates if you have recency of practice issue then working under supervision is an option for addressing this matter. A key point of this standard is to ensure that doctors who are not recent enough in their practice are given some oversight to return to work.
So in theory this means that if you are applying for a resident or registrar (trainee) role recency of practice should not really be an issue from a registration standpoint. But as we have highlighted above it may cause a problem in terms of your candidacy versus other candidates who do have recency of practice.
Option 2. Gain some clinical experience elsewhere to gain recency of practice
If working under supervision in Australia is not really an option for you then your next option is to regain clinical experience by working in another country. The Medical Board indicates that it considers clinical practice in overseas countries as meeting the standard of recency of practice.
This is generally an option for most IMGs and something I tend to recommend if they have been more than 2 years away from clinical medicine.
I will generally advise that you try to work for 3 months back in your own country, or another country where you have a registration, as this will then help you to both meet the Medical Board’s recency of practice standard as well as provide some reassurance to employers.
Are courses and observerships useful for recency of medical practice?
In a couple of words not really. Neither really helps that much.
Certainly, from a Medical Board perspective, observerships do not count as clinical practice towards the recency of practice requirement. Courses may be of assistance if you are required to undertake CPD relevant to your scope of practice.
From an employer’s perspective, a relevant course might help a fractional amount and an observership may also assist in a small way. The key benefit for an observership may be in being able to nominate a referee who has recent contact with you in the Australian health context. However, the merits of an observership are marginal compared to actual clinical practice.
Disclaimer. This post was written having researched the current standards for recency of practice. You should always consult an expert to gain individual advice on your circumstances, check out the official advice, and be mindful that guidelines and policies do change over time.
Related Questions.
Who Does Recency of Practice Apply to?
The recency of practice registration standard applies to all registered medical practitioners, except those with non-practising registration and recent graduates applying for provisional registration to undertake an accredited intern position.
Who Does Recency of Practice Not Apply to?
Recency of practice does not apply to non-practising clinicians or interns provisionally registered. It also does not apply to registered students.
Does Recency of Practice Only Affect International Medical Graduates?
No. The recency of practice standard affects all medical practitioners seeking registration or re-registration in Australia, including locally trained doctors.
What is Meant by Scope of Practice?
Scope of practice generally refers to the areas of medicine you are deemed fit to practice within.
If I Work More Than 38 Hours in a Week. Can I count These Additional Hours Towards Demonstrating Recency of Practice?
No. You may only accumulate 38 hours in one week. Additional time will not count towards the standard.
What If I Work Part-Time?
Doctors who work part-time must still complete the same minimum number of hours of practice – this can obviously be completed part-time over more weeks, for e.g. working 20 hours per week for 8 weeks of the year would meet the standard.
Will Doing a Certain Course Help My Recency of Practice?
From a Medical Board perspective courses and degrees do not assist in any way with the recent of practice standard. From an employer perspective, they might assist in a very marginal way but really nothing beats recent clinical practice.
Will Doing an Observership Help My Recency of Practice?
From a Medical Board perspective, observerships do not count as clinical practice towards recent of practice. From an employer perspective, an observership may assist in a small way. The key benefit may be in being able to nominate a referee who has recent contact with you in the Australian health context. However, the merits of an observership are marginal compared to actual clinical practice.
Does Overseas Experience Count?
Absolutely. The Medical Board “accepts practice outside Australia for the purposes of meeting the recency of practice registration standard.”






Hi Anthony,
I am planning to take the AMC MCQ next year. I am an OBGYN specialist with 10 years of experience but have not practiced since I moved here in Australia almost 6 years ago. My plan is to get an RMO job after I pass the MCQ. I don’t think that my experience will even matter as it is focused on women’s health. Will I have a chance at all of landing an RMO Job since as I understand it will be under supervision anyway? What are the odds?
Hi I am going to be transparent with you as I try to be with all IMGs who contact me.
The lack of any clinical experience for more than 6 years combined with being specialised for 10 years is going to be a real barrier for you in the job market when competing for RMO jobs.
There are some things you can do to improve your chances but its important to be realistic.